The momentum for including the public in the work to improve healthcare is gaining speed.
A bit of history
Around 2010 in Canada, we started to see Patient and Family Advisors (PFAs) at local hospitals become popular. Resident and Family Councils have been in place in long-term care facilities in many provinces and territories for even longer. And more recently we see citizen councils at local health authorities, at quality councils, at health professional bodies, and other types of health organizations.
In research, we started to see patient partners on research teams promoted by the Strategy for Patient-Oriented Research (SPOR). Read more.
Some disease-based organizations have had active groups of patients for years. Some examples, HIV/AIDs, and mental health.
Around 2018, the term “patient partner” becoming more widely used for PFAs.
We can learn from each other. And we can help embed the practice of involving the public in working toward a better future for the health and wellness of Canadians.
Structures of Patient Engagement & Partnership
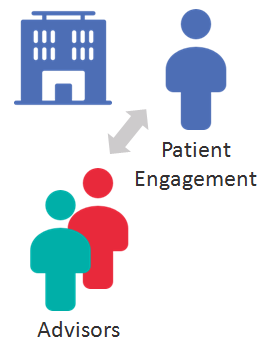
Patient partners are invited by healthcare organizations to join in the work to improve healthcare. Here are the two main models for how patient partners are managed:
The Main Type
In many cases, healthcare organizations have a “Patient Engagement” representative member or group. This team or person may have a different title, but their main goals are to:
- Recruit patient partners
- Orient partners to the organization
- Prepare and support staff while working with partners– take requests from internal working groups
- Assign patient partners within the organization
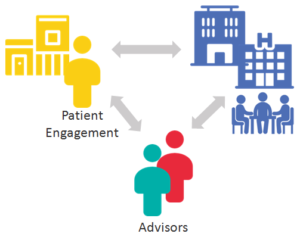
A Secondary Type
Some organizations arrange a roster of patient partners to make them available to other organizations or groups. These organizations arrange all the patient engagement functions on behalf of what they refer to as their clients.
In British Columbia, the Patient Voices Network administered by the BC Patient Safety & Quality Council is a good example of this. It provides advisors on request for many healthcare organizations and groups throughout BC.
Health Excellence Canada (HEC), is another example where the pool of advisors is used for healthcare clients. Increasingly, health authorities also have pools.
Since the start of the SPOR initiative in 2011, research teams have more and more welcomed patient partners on to their research teams. Often these are people the researchers know. Or researchers may go to their regional SPOR unit for patient partners.
Patient partners in research are not the same as patient participants who provide their data to the research team for analysis.
The Practices of Patient Engagement
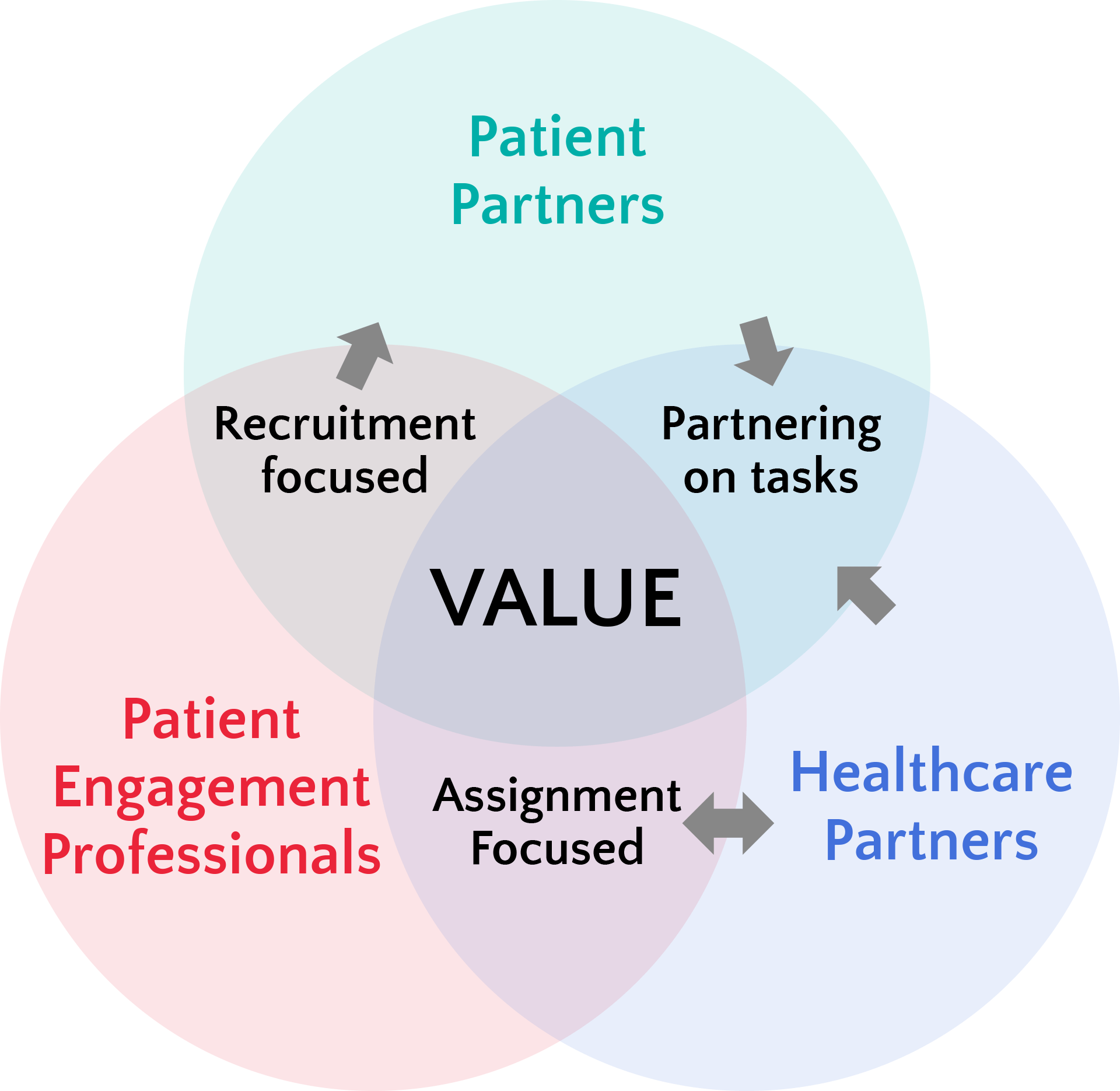
Traditionally when hospitals, health authorities and other healthcare organizations involve patient partners, they create
- a pool of patient and family advisors (patient partners)
- a Patient and Family Advisors Council (PFAC)
- or both a pool and PFAC
And they dedicate patient engagement staff to recruit, manage and assign the patient partners.
This is the practice of engaging patients.
For patient partners and the healthcare partners they collaborate with, their focus is the work they do together. This can be project work where there are a couple of patient partners on the team. Or it can be the PFAC or council where projects are brought to the council for consultation.
This is the practice of collaborating as a patient partner with healthcare partners.
To support these collaborations, the healthcare partners may be trained by the patient engagement professionals.
PAN was formed to provide a place for current and potential patient partners to support and learn from each other about the practice of collaborating.
This is the practice of fostering an engagement ready environment.
Patient engagement professionals may advise their organization on policies to support patient engagement. They may also educate decision-makers and those collaborating directly with patient advisors.